
Age Related Macular Degeneration (AMD)
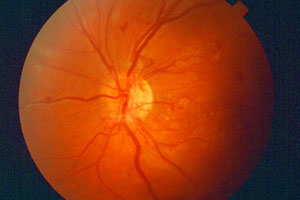
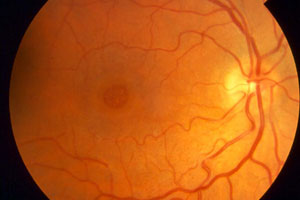
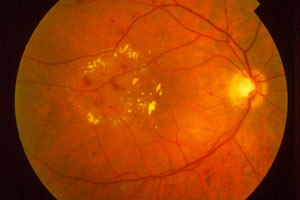
AMD is the leading cause of new cases of blindness in patients over 60 years of age. It is a degenerative disease of the macula which is the central part of the retina and affects the central vision. There are two forms of macular degeneration:
AMD is the leading cause of new cases of blindness in patients over 60 years of age. It is a degenerative disease of the macula which is the central part of the retina and affects the central vision. There are two forms of macular degeneration:
Dry AMD, or nonexudative AMD, where yellow white deposits called drusen accumulate in the deep macula with or without atrophy or ‘balding’ of the layers of the retina/macula. This leads to interference in the function of the photoreceptors responsible for processing of light coming into the eye which in turn causes decrease in vision. This dry AMD can progress to a more severe Wet AMD or exudative type of macular degeneration where abnormal choroidal vessels leak fluid, or rupture and bleed causing severe and often permanent central visual loss.
Read more about macular degeneration from Dr. Sastry’s ‘Ask the Expert Interview’
Diabetic Retinopathy
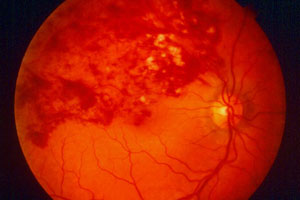
Diabetic retinopathy is an eye disease which affects persons with diabetes. It is the leading cause of new cases of blindness over all ages groups. Diabetes weakens the lining of the blood vessels in the retina causing leaking of fluid, lipid (cholesterol) and blood into the retina and macula. It also causes decrease in circulation to the retina (ischemia). In more advanced stages diabetes leads to abnormal new vessels called neovascularization which can rupture, bleed and stimulate scar tissue formation with retinal detachment.
Diabetic retinopathy is an eye disease which affects persons with diabetes. It is the leading cause of new cases of blindness over all ages groups. Diabetes weakens the lining of the blood vessels in the retina causing leaking of fluid, lipid (cholesterol) and blood into the retina and macula. It also causes decrease in circulation to the retina (ischemia). In more advanced stages diabetes leads to abnormal new vessels called neovascularization which can rupture, bleed and stimulate scar tissue formation with retinal detachment.
Branch Retinal Vein Occlusion (BRVO)
BRVO is a retinal vascular disease most often related to hypertension, elevated lipids/triglyceride/cholesterol, diabetes, carotid artery disease, cardiac disease, or hematologic (blood) disorders. In BRVO there is an occlusion of a branch retinal vein by a compressing, sclerotic retinal artery. This often leads to hemorrhage (bleeding), edema (swelling), or ischemia (poor circulation) of the retina and macula with resultant visual loss.
BRVO is a retinal vascular disease most often related to hypertension, elevated lipids/triglyceride/cholesterol, diabetes, carotid artery disease, cardiac disease, or hematologic (blood) disorders. In BRVO there is an occlusion of a branch retinal vein by a compressing, sclerotic retinal artery. This often leads to hemorrhage (bleeding), edema (swelling), or ischemia (poor circulation) of the retina and macula with resultant visual loss.

Central Retinal Vein Occlusion (CRVO)
CRVO is also a retinal vascular disease but involves occlusion of the main central retinal vein. Vascular, hematologic, and cardiac disease may predispose individuals to develop CRVO which leads to leakage of blood and fluid into the retina. In many cases the resultant poor circulation (ischemia) can lead to abnormal blood vessel formation in the iris (rubeosis) with painful increases in eye pressure (neovascular glaucoma).
CRVO is also a retinal vascular disease but involves occlusion of the main central retinal vein. Vascular, hematologic, and cardiac disease may predispose individuals to develop CRVO which leads to leakage of blood and fluid into the retina. In many cases the resultant poor circulation (ischemia) can lead to abnormal blood vessel formation in the iris (rubeosis) with painful increases in eye pressure (neovascular glaucoma).
Retinitis Pigmentosa (RP)
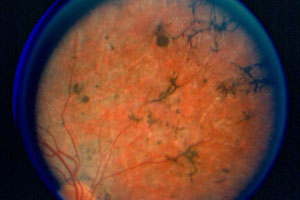
RP is a retinal degeneration, often hereditary, which affects the photoreceptors (rods and cones) which are the light sensing receptors. Usually, but not always, the rod receptors are affected first causing progressive decrease vision during dark hours, that is ‘night blindness’. There is also loss of peripheral vision leading to tunnel vision. As research into the genetics evolve we are learning more about RP as a spectrum of a number of related retinal degenerations some of which are associated with other disabilities like hearing loss. Most cases of RP are chronic and progress very slowly over decades.
RP is a retinal degeneration, often hereditary, which affects the photoreceptors (rods and cones) which are the light sensing receptors. Usually, but not always, the rod receptors are affected first causing progressive decrease vision during dark hours, that is ‘night blindness’. There is also loss of peripheral vision leading to tunnel vision. As research into the genetics evolve we are learning more about RP as a spectrum of a number of related retinal degenerations some of which are associated with other disabilities like hearing loss. Most cases of RP are chronic and progress very slowly over decades.
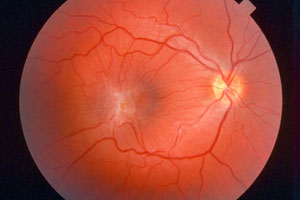
Macular Pucker
Macular Puckers develop as a result of contracture of an abnormal scar tissue membrane (epiretinal membrane, ERM) which grows over the surface to the macula. This causes wrinkling of the macula and subsequent distortion of central vision. These ERMs may grow as a result of aging, diabetes, trauma, inflammation, or previous eye surgery.
Macular Puckers develop as a result of contracture of an abnormal scar tissue membrane (epiretinal membrane, ERM) which grows over the surface to the macula. This causes wrinkling of the macula and subsequent distortion of central vision. These ERMs may grow as a result of aging, diabetes, trauma, inflammation, or previous eye surgery.
Macular Hole
A macular hole is a small opening in the central tissue of the retina called the macula. This area is responsible for our central vision or our driving, reading, recognizing people’s faces vision. Risk factors for the development of macular holes include: aging, trauma, or previous macular hole in the other eye.
A macular hole is a small opening in the central tissue of the retina called the macula. This area is responsible for our central vision or our driving, reading, recognizing people’s faces vision. Risk factors for the development of macular holes include: aging, trauma, or previous macular hole in the other eye.
Posterior Vitreous Detachment
With age the vitreous, the gel which fills the cavity in front of the retina, begins to liquefy and shrink. This normal for age process usually starts between 45 and 55 years of age. Individuals who are undergoing this process may briefly see floaters and even flashing lights in their vision. These symptoms usually subside and may leave a small residual floater in the vision. Rarely, a PVD may lead to a retinal tear or hole.
With age the vitreous, the gel which fills the cavity in front of the retina, begins to liquefy and shrink. This normal for age process usually starts between 45 and 55 years of age. Individuals who are undergoing this process may briefly see floaters and even flashing lights in their vision. These symptoms usually subside and may leave a small residual floater in the vision. Rarely, a PVD may lead to a retinal tear or hole.
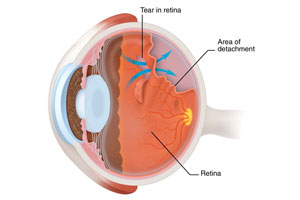
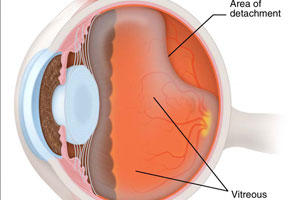
Retinal Detachment
Retinal Detachments occurs as a result of vitreoretinal traction where the gel filling the eye, called the vitreous, pulls and tugs of a tear of the retina, usually in the periphery. This allows fluid to perculate thru the tear, with subsequent detaching of the retina (analogous to wall paper coming off a wall). It is not known why some people get retinal detachments however, there are many risk factors including increasing age (with liquefication of the vitreous gel), diabetes, high myopia (near sightness), inflammation, and of course trauma.
Retinal Detachments occurs as a result of vitreoretinal traction where the gel filling the eye, called the vitreous, pulls and tugs of a tear of the retina, usually in the periphery. This allows fluid to perculate thru the tear, with subsequent detaching of the retina (analogous to wall paper coming off a wall). It is not known why some people get retinal detachments however, there are many risk factors including increasing age (with liquefication of the vitreous gel), diabetes, high myopia (near sightness), inflammation, and of course trauma.
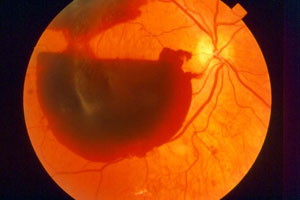
Retinal Hemorrhage
Bleeding or hemorrhage in the retina occurs when the blood vessels in the retina leak or rupture. Common causes include: diabetes, high blood pressure, blood disorders, cardiovascular problems, trauma, or aging.
Bleeding or hemorrhage in the retina occurs when the blood vessels in the retina leak or rupture. Common causes include: diabetes, high blood pressure, blood disorders, cardiovascular problems, trauma, or aging.
Macular Edema
Swelling in the macula (edema) results from fluid build up and thickening within the layers of retinal tissue. Tiny blood vessels which surround the macula are usually responsible for the leakage. Many disorders including diabetes, vein occlusions, uveitis (inflammation), and cataract surgery can cause macular edema. Depending on the cause there are different treatments which may include eye drops, steroid injections, laser treatment, or if vitreoretinal tractional is present vitreous surgery.
Swelling in the macula (edema) results from fluid build up and thickening within the layers of retinal tissue. Tiny blood vessels which surround the macula are usually responsible for the leakage. Many disorders including diabetes, vein occlusions, uveitis (inflammation), and cataract surgery can cause macular edema. Depending on the cause there are different treatments which may include eye drops, steroid injections, laser treatment, or if vitreoretinal tractional is present vitreous surgery.
